Let’s be honest, the phrase “root canal” doesn’t exactly conjure up images of rainbows and butterflies, does it? For many, it’s a term shrouded in mystery and a fair bit of dread. We’ve all heard the jokes, the horror stories whispered in waiting rooms. But what if I told you that the root canal is one of modern dentistry’s greatest unsung heroes? What if this much-maligned procedure is, in fact, a remarkable feat of medical engineering designed to do one thing and one thing only: save your natural tooth.
Think of it like this. Your tooth isn’t just a hard, white chunk of enamel. It’s a living, breathing organ with a complex internal structure. Deep inside, beneath the layers of enamel and dentin, lies the pulp—a soft tissue housing nerves, blood vessels, and connective tissue. This pulp is the tooth’s life source during its development. But once the tooth is fully mature, it can survive without it, getting its nourishment from the surrounding tissues. The problem arises when this inner sanctum, the pulp, becomes infected or inflamed.
So, what happens then? Well, you have two main choices. You can let the infection rage on, leading to unbearable pain, an abscess (a pocket of pus that forms at the root tip), and eventually, the complete loss of the tooth. Or, you can call in the cavalry: the root canal treatment. This procedure isn’t about causing pain; it’s about ending it. It’s a rescue mission, meticulously planned and executed to salvage a tooth that would otherwise be doomed.
In this article, we’re going to pull back the curtain. We’ll walk through the entire process, demystify the jargon, and show you exactly how this incredible treatment works to preserve your natural smile. By the end, you might just see the root canal in a whole new light—not as a dental villain, but as a true superhero.
Why Would a Tooth Need Saving? The Usual Suspects
First, let’s talk about why the pulp, that inner core of your tooth, might throw in the towel. How does it get infected or inflamed in the first place? It’s usually one of a few common culprits:
- Deep Decay: This is the big one. A cavity might start as a tiny spot, but if it’s left unchecked, it can burrow its way through the enamel and dentin, right into the pulp. It’s like leaving a door open for bacteria to march straight into the tooth’s command center.
- Cracks or Chips: A significant crack in a tooth can provide a direct highway for bacteria to reach the pulp. Even a tiny, hairline crack can be enough to cause big problems.
- Repeated Dental Procedures: Sometimes, a tooth that has had several large fillings or other work might simply become stressed over time. The trauma from these procedures can eventually cause the pulp to become inflamed.
- Trauma: A blow to the face might damage the pulp even if the tooth doesn’t have a visible crack. The injury can disrupt the blood supply to the pulp, leading to its slow death.
When the pulp gets infected, your body sends out an SOS in the form of pain. You might experience a throbbing toothache, sensitivity to hot and cold that lingers, pain when you chew or apply pressure, or even swelling in your face or gums. Ignoring these signals is like ignoring a fire alarm. The infection won’t just go away; it will spread, potentially leading to a serious abscess and systemic health issues. To learn more, visit Indental Castle Hill through the following link: https://maps.app.goo.gl/
The Root Canal Rescue Mission: A Step-by-Step Guide
So, how does a root canal treatment actually save the day? Let’s break down the process. It’s far more sophisticated than just “drilling a hole.” It’s a precise, delicate procedure that requires skill and care.
Step 1: Diagnosis and the Blueprint
It all starts with a proper diagnosis. Your dentist will examine the tooth, take X-rays, and likely perform a few tests (like tapping on the tooth or applying cold) to confirm that the pulp is indeed the source of the problem. Those X-rays are crucial—they act as a blueprint, showing the dentist the number, shape, and length of the root canals. You see, teeth aren’t uniform. Front teeth typically have one root canal, while molars can have two, three, or even more. Knowing the exact layout is the first step to a successful mission.
Step 2: Comfort is Key – Local Anesthesia
This is where we bust the biggest myth of all: that root canals are excruciating. The truth is, the procedure itself is done to relieve the pain caused by the infection. Your dentist will numb the area completely with a local anesthetic. You’ll be awake, but you shouldn’t feel any pain during the procedure—maybe just some pressure or movement. The goal is to make you as comfortable as possible.
Step 3: Access and the Clean-Out
Once you’re numb, your dentist will place a small protective sheet called a “dental dam” over the tooth to isolate it, keeping it clean and dry during the procedure. Then, a very small opening is made in the crown (the top part) of the tooth to access the pulp chamber. This is the gateway.
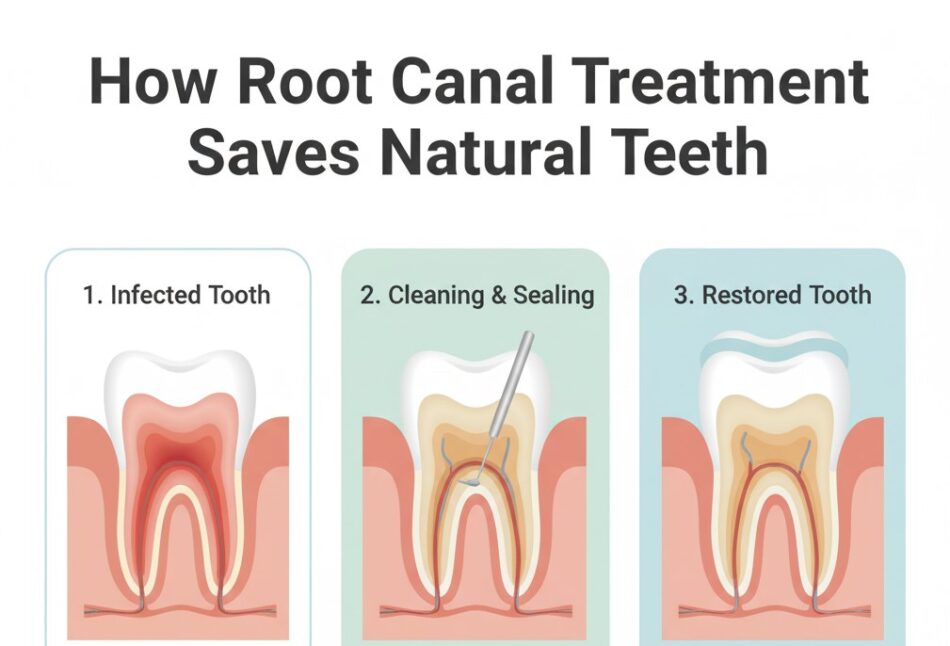
Using incredibly fine instruments, the dentist then carefully removes the diseased or dead pulp tissue from inside the pulp chamber and the root canals. This is the core of the “rescue.” Think of it like cleaning out a badly infected wound. We’re removing the source of the problem—all the bacteria and decayed nerve tissue.
Step 4: Shaping, Disinfecting, and Flushing
After the pulp is removed, the canals need to be shaped and meticulously cleaned. Your dentist will use small files to gently enlarge and smooth the canals. This isn’t just a quick scrub; it’s a thorough cleaning process. The canals are flushed with special antibacterial and antiseptic solutions to kill any remaining bacteria and wash away any debris. This step is critical to prevent re-infection down the line.
Step 5: The Final Seal – Filling the Canals
You can’t leave a clean, hollow space inside your tooth. It would be like cleaning a house and then leaving the front door wide open for new pests to wander in. So, once the canals are perfectly clean and dry, they are filled with a biocompatible material, usually a rubber-like substance called gutta-percha. This material seals the canals, preventing bacteria from re-entering. The access opening in the crown is then closed with a temporary filling.
Step 6: The Crowning Glory – The Final Restoration
A root canal-treated tooth is saved, but it’s also more fragile than a living tooth. The process of accessing and cleaning it removes a significant amount of the tooth’s structure. Because of this, the tooth often needs a permanent crown (cap) to be placed over it. This crown acts like a protective helmet, restoring the tooth’s strength, shape, and appearance, and allowing you to chew normally again. It’s the final, crucial step in the restoration process, ensuring your saved tooth can last a lifetime.
Root Canal vs. Extraction: Why Saving the Tooth is Almost Always Better
Now, you might be thinking, “Wouldn’t it be easier to just pull the tooth? One quick tug and the problem is gone, right?” It’s a fair question, but extraction is rarely the better long-term option. Pulling a tooth is like demolishing a house because of a faulty plumbing system. It solves the immediate problem but creates a whole new set of challenges.
The Consequences of an Extraction:
- The Domino Effect: Your teeth are a team. They rely on each other for support. When one tooth is removed, the adjacent teeth can start to shift or tilt into the empty space. This can lead to misalignment, bite problems, and difficulties with cleaning, which in turn can cause decay and gum disease in the other teeth. It’s a domino effect that can compromise your entire smile.
- Bone Loss: Your jawbone needs the stimulation from your tooth roots to maintain its density and strength. When a tooth is extracted, that area of the bone no longer receives that stimulation and begins to deteriorate or resorb over time. This can change the shape of your face, leading to a sunken appearance, especially if multiple teeth are missing.
- The Cost of Replacement: An extraction might seem cheaper upfront, but then you’re left with a gap. To properly replace that tooth, you’re looking at either a dental bridge (which involves grinding down the healthy teeth on either side of the gap) or a dental implant (a surgical procedure that is often more expensive and time-consuming than a root canal itself).
The Benefits of a Root Canal:
- You Keep Your Natural Tooth: This is the biggest win. It maintains the natural structure of your jaw and bite.
- Efficient Chewing and Normal Bite Force: A restored tooth after a root canal functions just like a natural tooth.
- Natural Appearance: With a crown, the tooth looks completely normal.
- Protects Other Teeth: It prevents the shifting and problems associated with a gap.
- It’s Cost-Effective: When you consider the long-term costs of replacing an extracted tooth, a root canal and crown are often the more economical choice.
To make the comparison crystal clear, let’s look at this side-by-side:
Root Canal Treatment vs. Tooth Extraction: A Clear Comparison
| Feature | Root Canal Treatment | Tooth Extraction |
|---|---|---|
| Primary Goal | Save the natural tooth | Remove the problematic tooth |
| Pain Level | Minimal during procedure (due to anesthesia); relieves pre-existing pain | Minimal during procedure; post-extraction soreness |
| Procedure Time | Typically 1-2 appointments | Usually one quick appointment |
| Long-Term Oral Health | Preserves bone, prevents teeth shifting, maintains bite | Can lead to bone loss, teeth shifting, and bite issues |
| Aesthetics | Tooth is restored with a crown, looking natural | Leaves a gap that requires a bridge, implant, or denture |
| Cost Over Time | One-time cost for saving the tooth | Initial extraction cost + ongoing cost for replacement |
| Functionality | Restores full chewing ability | Chewing ability is compromised until the tooth is replaced |
Debunking the Myths: Setting the Record Straight
It’s time to tackle those persistent root canal myths head-on.
- Myth 1: Root Canals Are Painful. This is the granddaddy of them all. With modern anesthesia and techniques, a root canal is no more uncomfortable than getting a standard filling. The pain people associate with root canals is actually the pain of the infection before the procedure. The treatment is the solution to that pain.
- Myth 2: It’s Better to Pull the Tooth. As we’ve just explored, nothing is as good as your natural tooth. Dentists are in the business of saving teeth, and a root canal is the premier way to do that. Extraction is a last resort.
- Myth 3: A Root Canal “Kills” the Tooth. Technically, yes, the nerve tissue is removed, so the tooth loses its sensitivity to hot and cold. But the tooth itself is very much alive and functional, held securely in your jawbone by the periodontal ligament. It’s more accurate to say the root canal removes the diseased part and allows the healthy structure to remain.
The Aftermath: Caring for Your Saved Tooth
So, you’ve had the root canal and the crown placed. What now? The great news is that caring for a root-canaled tooth isn’t much different from caring for your other teeth. It can still be susceptible to decay, and the gums around it still need to be healthy. So, your routine remains the same: brush twice a day, floss daily, and see your dentist for regular check-ups and cleanings. Your saved tooth has been given a second chance, and with proper care, it can serve you well for the rest of your life.
Conclusion
The next time you hear “root canal,” I hope you’ll think differently. See it not as a procedure to be feared, but as a sophisticated, life-saving intervention for your tooth. It’s a testament to how far dentistry has come—a field that prioritizes preservation and health. It’s a proactive, intelligent choice that honors the incredible engineering of your natural teeth.